Introduction:
Follicular lymphoma (FL) is the most common indolent non-Hodgkin lymphoma and accounts for nearly a quarter of cases. As a heterogenous disease with an estimated 20% having progression of disease within 24 months of first FL therapy, FL often quickly becomes relapsed or refractory (R/R) to current therapy. The objective of this study was to evaluate the real-world treatment patterns, time to next treatment, and associated costs and healthcare resource utilization (HCRU) in patients with FL in the United States.
Methods:
A retrospective observational study was conducted using an integrated real-world database including linked data from the Symphony Integrated Dataverse (IDV ®), electronic medical records, specialty pharmacy, and in-office dispensing datasets. Patients were included in the study if they were ≥ 18 years old and initiated a first-line (1L), second-line (2L), third-line (3L), or fourth-line (4L) of therapy for FL between 1/1/2019 and 12/31/2022. Patients were categorized by line of therapy into non-mutually exclusive cohorts based on the date of initiation of their treatment regimen. Each line of therapy cohort was followed for a minimum of 90 days through lost to follow-up or end of the study period (3/31/2023). Patients were also required to have continuous pre-index enrollment of 365 days to record baseline comorbidities. Demographics, clinical characteristics, and treatment regimens were examined for each line of therapy cohort. Within each line of therapy, patients were categorized into 6 mutually exclusive subgroups based on their treatment regimens: bendamustine + rituximab (BR), rituximab monotherapy (R-mono), cyclophosphamide, doxorubicin, prednisone, rituximab + vincristine (R-CHOP), bendamustine + obinutuzumab (BO), lenalidomide + rituximab (R2), and other treatments for all other regimens. Advancement to the next line of therapy, treatment regimen distribution, and switching for each cohort and subgroup were evaluated during the follow-up period. Treatment duration, time to next treatment (TTNT), HCRU and pharmacy costs were measured for each cohort and treatment regimen during the follow-up period. HCRU included outpatient visits and hospital claims, reported as per patient per month (PPPM) over the time on each treatment regimen.
Results:
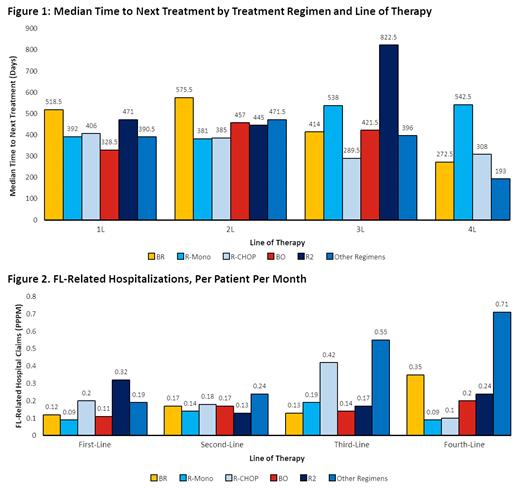
The study population included 9,579 patients initiating 1L, and then 3,061, 952 and 263 patients who received 2L, 3L, and 4L, respectively. The median follow-up was 719 days (1L), 652 days (2L), 578 days (3L), and 468 (4L). Mean age at index was similar across treatment lines, ranging from 66.7 years (1L) to 67.9 years (4L). Males represented a little under half (47.3%) in 1L cohort but increased slightly with subsequent lines (49.3%, 2L; 54.9%, 3L; 70% 4L). The most common baseline comorbidities across treatment lines were hypertension (1L=35.2%; 2L=32.3%; 3L=29.8%; and 4L=28.1%) and gastrointestinal disease (1L=23.9%; 2L=22.2%; 3L=22.2%; and 4L=22.1%). Across all treatment lines, R-mono was the most common regimen (1L=34.1%; 2L=29.0%; 3L=23.8%; and 4L=18.6%) followed by BR (1L=32.8%; 2L=17.3%; 3L=12.0%; and 4L=11.4%), and R-CHOP (1L=14.5%; 2L=12.8%; 3L=10.1%; and 4L=9.5%). Median TTNT across all regimens was 417 days (159, 691) in 1L, 444.5 days (225, 661) in 2L, 414 days (174, 784) in 3L, and 382.5 days (200.5, 599.5) in 4L (Figure 1). Mean (standard deviation; SD) of all-cause outpatient visits PPPM were 5.99 (4.86) in 1L, 6.06 (5.42) in 2L, 6.27 (6.04) in 3L, and 6.25 (5.95) in 4L. Mean (SD) of FL-specific outpatient visits PPPM were 4.59 (4.00) in 1L, 4.49 (4.31) in 2L, 4.57 (4.93) in 3L, and 4.42 (4.65) in 4L. The mean all-cause hospitalizations PPPM were 0.35 (1.72) in 1L, 0.79 (3.36) in 2L, 1.94 (6.29) in 3L, and 1.85 (5.00) in 4L. The mean FL-related hospitalizations PPPM were 0.13 (0.76) in 1L, 0.18 (1.02) in 2L, 0.36 (1.56) in 3L, and 0.45 (2.12) in 4L (Figure 2). Average pharmacy costs PPPM increased from $1,033 ($3,963.8) in 1L to $2,166.6 ($6,001.1) in 2L, and $2,943.7 ($6,413.1) to $3,374.1 ($7,361.3) in 3L and 4L, respectively.
Conclusions:
Real-world treatment patterns for patients with FL were shown to be mostly consistent with clinical guidelines. This study highlighted that TTNT decreased while hospitalizations and pharmacy costs increased as line of therapy progressed, suggesting high financial burden and unmet need for better treatment options for R/R FL patients.
Disclosures
Shah:Incyte, Jazz Pharmaceuticals, Kite/Gilead, SERVIER: Research Funding; Moffitt Cancer Center: Current Employment; DSMC, Pepromene Bio: Membership on an entity's Board of Directors or advisory committees; Pharmacyclics/Janssen, Spectrum/Acrotech, BeiGene, Gilead Sciences: Honoraria; Celgene, Novartis, Pfizer, Janssen, Seattle Genetics, AstraZeneca, Stemline Therapeutics, Kite/Gilead: Other: Travel, Accommodations, Expenses; Takeda, AstraZeneca, Adaptive Biotechnologies, BMS/Celgene, Novartis, Pfizer, Amgen, Precision Biosciences, Kite/Gilead, Jazz Pharmaceuticals, Century Therapeutics, Deciphera, Autolus Therapeutics, Lilly, Pepromene: Consultancy. Xue:BeiGene USA: Current Employment. Seymour:Flatiron Health: Ended employment in the past 24 months; Roche: Current equity holder in publicly-traded company; BeiGene: Current Employment, Current equity holder in publicly-traded company. Furnback:Real Chemistry, Inc: Current Employment, Current equity holder in publicly-traded company. Chuang:Real Chemistry, Inc: Current Employment. Yang:BeiGene: Current Employment, Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees, Other: Travel, Accommodations, Expenses, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal